3 ALTERNATIVES TO
NSAIDS AND OTHER DRUGS
I admit the following methods are decidedly unsexy.
Unlike the latest and greatest pharmaceutical, these take a bit of work, a bit of time, and they certainly aren’t going to make anyone millions. They also don’t come with any nasty side effects besides a better mood, better overall health, and more energy.

First, let’s talk a little about how our brains process pain. Let’s say your knee hurts. You think, “There is something wrong with my knee that is causing me pain.” Maybe. Your brain is receiving sensory and proprioceptive input, and in turn it is sending a sensation of pain down to your knee. But, is your experience of pain proportional to the level of dysfunction in your knee?
Maybe you do have some sort of biomechanical imbalance that is causing your knee to be stressed in a way for which it is not designed, resulting in inflammation or damage in the joint. Maybe you have a trigger point in your hip referring pain down into your knee. Maybe the afferent signal from your knee is too strong, or your central pain inhibitory mechanisms are too weak, or your pain sensitivity is too high due to stress or emotional factors. Pain is complex, and there are many points along this signaling pathway that can alter your pain levels.
One thing we do know: inflammation ratchets up pain levels.
We know this is true acutely: red, swollen injuries are often very painful. Acute inflammation is a natural response to trauma and injury. It is a necessary part of the healing process; ideally your body heals the injury and inflammation levels return to normal. However, problems arise when this inflammation ceases to be an acute response and turns into a systemic one, when it becomes a low-level feature of your physiology that’s always on and perpetually engaged. This is a problem because chronic inflammation is also linked to chronic pain.
Chronic inflammation has been associated with many painful conditions such as arthritis and chronic musculoskeletal injuries. C-Reactive Protein (CRP) has recently received attention as a marker of chronic inflammation, and research has shown that there is a connection between chronic pain and CRP levels (1). Specifically, pain perception may be higher in those with elevated CRP levels. In a study of 99 pairs of twins, elevated levels of CRP were associated with lower pain thresholds and increased pain sensation (2). Similarly, a study of cancer patients showed CRP was significantly correlated with perceived pain (3). Since systemic inflammation may contribute to the development and maintenance of pain conditions, by reducing inflammation, we may be able to decrease pain. So, how do we do this?
1. Tweak Your Diet
The best way to control systemic inflammation is through your diet. The tricky part is determining what is inflaming to you and eliminating it. This differs from person to person, but here are some likely culprits:
- Excessive refined sugar intake, especially sugar-sweetened beverages, may increase inflammation (4)
- Grains, especially gluten, may be inflammatory; joint pain has been linked to gluten intolerance. (5)
- Omega 6 oils: higher circulating levels of an inflammatory cytokine, IL-6, is a highly significant predictor of knee osteoarthritis (6). Excess Omega 6 polyunsaturated fat intake (found in corn, soybean, canola oil) leads to higher levels of IL-6.
- Dairy, especially milk, may be inflammatory for some people.
- Nightshades like potatoes, eggplants, tomatoes, and peppers contain a chemical alkaloid called solanine, which may increase inflammation and pain, particularly in those with arthritis.
Instead, focus on anti-inflammatory foods such as:
- Brightly colored fruits and vegetables, especially dark leafy greens, cruciferous vegetables, berries, onions and shallots
- Spices like turmeric, garlic, ginger, rosemary, oregano
- Omega 3 fatty acids: cold water oily fish like salmon, grass-fed meat and butter, pastured eggs
- Other healthy fats like olive oil, coconut oil, avocado, nuts, and seeds
2. Prioritize Sleep
Inadequate sleep is not only a consequence of pain, but it is also likely to play an integral role in the expression of pain. It is also linked to inflammation. Most people need somewhere around 8 hours of sleep each night. Maybe you need less or more—the main question is whether you feel rested upon waking. Sleep disturbance is increasingly recognized as a direct contributor to both increased pain sensitivity and impaired endogenous pain modulation (how your brain regulates pain).
- Sleep studies have found elevated inflammatory markers (including CRP) in response to prolonged sleep loss, and sleep disturbance positively correlates with clinical pain severity (7,8,9).
- Fortunately, napping seems to reverse the increased pain sensitivity (10) and inflammatory biomarkers (11) following a poor night of sleep. So if you can’t get a good night’s sleep, at least allow yourself to take a nap the next day.
3. Get Some Acupuncture
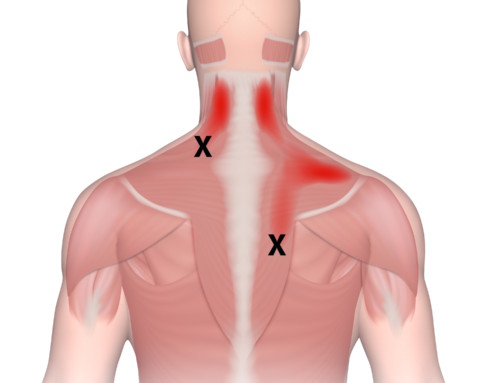
Acupuncture is very effective at treating pain for a number of reasons: it has an anti-inflammatory effect in the body, it releases endorphins (our own natural painkillers), it relieves muscle spasms, and it releases trigger points that refer pain (12).
- In an extensive analysis, data from nearly 18,000 individuals involved in 29 high-quality clinical trials revealed that acupuncture is associated with improved pain outcomes compared with controls, and is an effective treatment for chronic back and neck pain, osteoarthritis, shoulder pain, and headaches (13).
- Ear acupuncture and acupressure in particular have been shown to be particularly effective in the treatment of pain. A 2015 study examining the efficacy of using auriculotherapy to treat chronic low back pain found a 56% reduction in pain intensity and a 26% improvement in physical function in the auriculotherapy group vs (9% and 2% in controls). The study often found a significant change in inflammatory and neuropeptide levels in the treatment group(14).
Of course, this is all connected. If you are in pain, maybe you don’t sleep very well, which not only increases inflammation, but also reduces your leptin levels (the hormone that suppresses hunger) and makes you more likely to indulge in unhealthy eating habits, which may further increase inflammation and pain levels…(15). Fortunately, acupuncture has a balancing effect on the whole body, and can be used to not only treat pain, but sleep and cravings as well:
- Acupuncture benefits sleep and reduces insomnia more effectively than estazolam—a common sleep medication. (16)
- Acupuncture has also been shown to have regulatory effects on leptin, the hormone that regulates hunger and cravings(17). This may make sticking to an anti-inflammatory diet easier.
Certainly, pain can run the gamut from annoying to exhausting or even debilitating. NSAIDS and even the more powerful drugs have their place in pain management; problems do arise, however, when we use these over long periods of time. This post is not meant to pass judgment on anyone using pain medications, but I hope it provides a fresh and potentially empowering perspective about ways in which we can manage an aspect of our physiology that so often seems beyond our control.
References:
- Briggs, Matthew S., et al. “Relations of C-reactive protein and obesity to the prevalence and the odds of reporting low back pain.” Archives of physical medicine and rehabilitation4 (2013): 745-752.
- Afari N, Mostoufi S, Noonan C, Poeschla B, Succop A, et al. (2011) C-reactive protein and pain sensitivity: findings from female twins. Annals of Behavioral Medicine 42(2): 277-283.
- Oliveira, K. G., et al. “Relationship of inflammatory markers and pain in patients with head and neck cancer prior to anticancer therapy.” Brazilian Journal of Medical and Biological Research7 (2014): 600-604.
- Aeberli, Isabelle, et al. “Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial.” The American journal of clinical nutrition2 (2011): 479-485.
- Castillo-Ortiz, José Dionisio, et al. “Anti-transglutaminase, antigladin and ultra purified anti-gladin antibodies in patients with a diagnosis of rheumatoid arthritis.” Reumatología Clínica (English Edition)1 (2011): 27-29.
- Livshits, Gregory, et al. “Interleukin‐6 is a significant predictor of radiographic knee osteoarthritis: The Chingford study.” Arthritis & Rheumatism7 (2009): 2037-2045.
- Meier-Ewert, Hans K., et al. “Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk.” Journal of the American College of Cardiology4 (2004): 678-683.
- Haack, Monika, Elsa Sanchez, and Janet M. Mullington. “Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers.” Sleep9 (2007): 1145.
- Mullington, Janet M., et al. “Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation.” Progress in cardiovascular diseases4 (2009): 294-302.
- Faraut, Brice, et al. “Napping reverses increased pain sensitivity due to sleep restriction.” PloS one2 (2015): e0117425.
- Faraut, Brice, et al. “Napping Reverses the Salivary Interleukin-6 and Urinary Norepinephrine Changes Induced by Sleep Restriction.” The Journal of Clinical Endocrinology & Metabolism3 (2015): E416-E426.
- Zijlstra, Freek J., et al. “Anti-inflammatory actions of acupuncture.” Mediators of inflammation2 (2003): 59-69.
- Vickers, Andrew J., et al. “Acupuncture for chronic pain: individual patient data meta-analysis.” Archives of internal medicine19 (2012): 1444-1453.
- Lin, Wei-Chun, et al. “The Anti-Inflammatory Actions of Auricular Point Acupressure for Chronic Low Back Pain.” Evidence-Based Complementary and Alternative Medicine 501 (2015): 103570.
- Taheri, Shahrad, et al. “Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index.” PLoS medicine3 (2004): e62.
- Guo, Jing, Lin-Peng Wang, Cun-Zhi Liu, Jie Zhang, Gui-Ling Wang, Jing-Hong Yi, Jin-Lian Cheng, and R. Musil. “Efficacy of acupuncture for primary insomnia: a randomized controlled clinical trial.” Deutsche Zeitschrift für Akupunktur 57, no. 4 (2014): 31-32.
- Güçel, Funda, et al. “Influence of acupuncture on leptin, ghrelin, insulin and cholecystokinin in obese women: a randomized, sham-controlled preliminary trial.” Acupuncture in Medicine3 (2012): 203-207.